Ulcerative Colitis
Ulcerative Colitis : Definition
Western Medicine
Ulcerative colitis (UC) is a chronic medical condition characterized by inflammation of the inner lining of the colon and rectum.
The inflammation usually begins in the rectum and lower intestine and spreads upward to the entire large intestine, which causes ulceration of the surface of the colon, and results in pus, mucus, and bleeding. The disease commonly starts gradually, with non-bloody diarrhea progressing to bloody diarrhea with symptoms slowly worsening over the course of a few weeks. In about 20 percent of patients, the initial attack of ulcerative colitis is associated with bloody diarrhea and other severe symptoms, with inflammation extending into the colon.
Ulcerative colitis commonly follows a chronic intermittent course, with long periods of remission interspersed with acute attacks lasting weeks to months.
Chinese Medicine
Ulcerative colitis (Colitis ulcerosa, UC) is a form of inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the large intestine. Based on characteristic signs like persistent diarrhea, rectal bleeding, fever, abdominal cramps and weight loss, TCM puts the chronic condition under the categories of "protracted diarrhea", "protracted dysentery", "bloody stools", or "organ intoxication".
In China, TCM treatment in the diagnosis of ulcerative colitis was first reported in 1958; however, similar clinical experiences can be tracked to a very early period. In the Han dynasty, the symptoms were recorded in a TCM classic, Jinkui Yaolue (Synopsis of the Golden Chamber), which proposed to treat ulcerative colitis by therapeutic approaches like detoxifying, cleansing, warming, astringing and consolidating. The author also formulated Pulsatilla Root Decoction (bai tou weng tong) and Peach Blossom Decoction (tao hua tang) specifically for the condition. This established an important foundation for exploring the mechanism of the disease and developing relevant treatment methods. Modern TCM after many years of clinical studies concluded that herbal administrations along with herbal enemas are a better way to control symptoms and can maintain a longer remission from the disease.

In respect to herbal usage, traditional prescriptions usually contain ingredients that fortify the spleen, replenish qi, clear heat and expel dampness. However, specialists have found that mere application of herbs to activate circulation and remove stasis can also achieve similar results.
Ulcerative colitis is a common and complex clinical condition, TCM treatment has its unique advantage.
In respect to herbal usage, traditional prescriptions usually contain ingredients that fortify the spleen, replenish qi, clear heat and expel dampness. However, specialists have found that mere application of herbs to activate circulation and remove stasis can also achieve similar results.
Ulcerative colitis is a common and complex clinical condition, TCM treatment has its unique advantage.
Ulcerative Colitis : Causes
Western Medicine
Ulcerative colitis primarily affects young adults, but it can occur at any age from five to eighty years and women tend to be more commonly affected than men. It is a worldwide disorder with high-incidence areas that include United Kingdom, the United States, northern Europe and Australia. Low-incidence areas include Asia, Japan, and South America.
The causes of ulcerative colitis remain unknown. The major theories include infection, allergy to food component, genetics, environmental factors, and immune response to bacteria or other antigens.
Infection
Although use of antibiotics has been shown to improve treatment of active ulcerative colitis, no specific bacteria or virus have been isolated despite many attempts; therefore ulcerative colitis is unlikely to be due to a simple infection. Organisms such as shigella and pathogenic E. Coli have been investigated as possible infectious agents but they have not been associated with the etiology of the disease.
Food Allergy
The majority of patients with ulcerative colitis are found to be sensitive to milk and this led to claims that food allerg ies , particularly to milk, were the cause of the disease. Although some studies suggest that about twenty percent of patients with ulcerative colitis can benefit from a milk-free diet, there is very little scientific evidence to prove dietary allergy as the etiology of ulcerative colitis.
Environmental Factors
Other environmental factors proposed as contributing factors in the etiology of ulcerative colitis are oral contraceptives and smoking. The use of birth control pills was found to be more common in women with ulcerative colitis compared to women without the disease. Many studies have shown that ulcerative colitis is more common in nonsmokers than in smokers. The risk of developing ulcerative colitis is shown to be highest for previously heavy smokers, especially within the first two years of cessation. Smoking has shown to alter the function of the cells in the inner lining of the colon but the exact mechanism of the protective effect of smoking is unknown.
Genetics
There is some evidence that support the theory that ulcerative colitis may be due to genetic factors. The relatives of patients with ulcerative colitis are more likely to have the same disease compared to the general population and approximately ten to twenty percent of patients affected also have at least one other family member with the same disease. Numerous genes with a possible association with ulcerative colitis have been identified. Possible mechanisms proposed for genetic factors contributing to the cause of ulcerative colitis include metabolic defects and connective tissue disorders.
Autoimmune Disease
The current leading theory suggests that ulcerative colitis is an autoimmune disease, where the body's own immune system triggers an inflammatory response against an antigen in the intestinal wall. In this theory, the patient's immune system mounts an immune response against an antigen, either food particles or microbial organisms which the immune cells recognize as foreign objects, and this immune response triggers inflammatory effects. However, because of similarities between proteins on the cells of the inner lining of the colon and the antigens (dietary or microbial), the patient's own immune system is activated against the cells on the surface of the colon. Once the immune cells are activated, inflammatory mediators are released which not only cause tissue damage but also amplify the immune response and promote further inflammation in the inner lining of the colon.
Chinese Medicine
Ulcerative colitis is a systemic disease that affects many parts of the body, although patients mainly manifest with intestinal symptoms. In TCM understanding, the problem is closely associated with organ dysfunction, in particular the spleen, that cause a failure to self regulate the intestinal environment. TCM specialists generally agree that constitutional weakness, invasion of exogenous pathogens, an unbalanced diet and emotional factors all contribute to the development of the problem. The pathogenesis is described below:
Damp-heat in the large intestine
In TCM theory, the large intestine is a hollow organ belonging to the digestive system; it receives the "impure" parts of digested food from the small intestine and continues to absorb water from these materials. At the end of the process, stools are formed and excreted through the anus. Digestive problems, whether resulting from either external or internal origin, tend to retain dampness in the intestines, and will further transform into damp-heat in the long run. When the damp-heat pathogens disturb the transmission process in the large intestine, diarrhea will occur; and if the intestinal membrane is irritated, the passing stools will have pus and blood.
Liver overacting spleen
In TCM, the liver promotes flowing and spreading movements, which is embodied in three functional aspects: regulating qi, regulating emotions and enhancing the digestive processes. Long-term emotional stimulation cause a state called "liver stagnation", not only making the blood and qi flows sluggish, but also interfering with the digestive functions in the spleen and stomach. This facilitates damp-heat to accumulate in the large intestine.
Spleen and kidney deficiencies
The spleen rules transformation and transportation, which means it is the primary organ in regulating digestion. On the other hand, the kidneys' warming and propelling activities enable the spleen to work properly. Deficiencies in these two organs lead to a chronic state, which causes intestinal problems such as persistent or intermittent diarrhea to occur.
Blood stasis and qi congestion
Long duration of diarrhea leads to a depletion of blood and qi, which cause pathological wastes to form inside the intestines. They can in turn act directly or indirectly on the organs, and give rise to more complex conditions.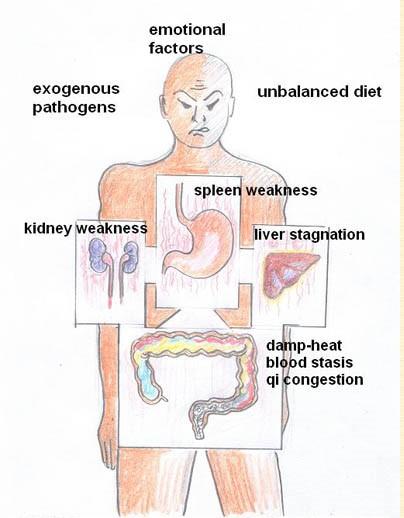
UC development from a TCM perspective.
Ulcerative Colitis : Symptoms
Western Medicine
Major symptoms of ulcerative colitis are diarrhea, rectal bleeding, the passage of mucus, and abdominal pain. The onset of symptoms is usually slow and insidious and often symptoms have been present for weeks or even months before patients seek medical help. Patients often experience frequent bowel movements of small volume and fecal incontinence. Other symptoms include fever, pain and weight loss.
In general, the severity of symptoms correlates with the severity of the disease. More generalized symptoms such as fever, fatigue, and weight loss are more common if inflammation is extended to all or most of the colon. If the disease is confined to the rectum, the only symptoms may be persistent desire to empty the bowel or spasm of the rectum with or without bloody diarrhea. Some patients, especially elderly patients or those with inflammation confined to the rectum, may complain of constipation and hard stools.
Classification of disease severity
Severity of disease is categorized as mild, moderate, or severe according to clinical symptoms.
- Mild: diarrhea and rectal bleeding are usually the only symptoms. Patients experience less than four stools daily, with or without blood.
- Moderate: typical symptoms are five or six bloody bowel movements per day and bloody diarrhea is often associated with large amount of mucus and pus. Incontinence is often a problem especially when the rectum is severely inflamed. Abdominal pain may also be present in addition to low-grade fever and fatigue.
- Severe: patients experience frequent episodes of bloody diarrhea (more than six bloody stools daily) and they may become anorectic and nauseated. In severe attacks, patients may vomit and experience symptoms of anemia such as breathlessness, ankle swelling, and fatigue. Weight loss, fever, fast heartbeat, dizziness, and severe cramping or abdominal pain can also occur with severe cases of the disease.
Other organ systems affected by ulcerative colitis
Mouth: oral ulcers occur in about ten percent of patient s with active ulcerative colitis.
Eyes: inflammation of the eyes occurs in approximately five to eight percent of patients with active ulcerative colitis. Corticosteroid eye drops are useful for controlling symptoms of inflammation.
Joints: in approximately ten to fifteen percent of patient s with an acute attack of ulcerative colitis, larger joints (knees, hips, ankles, wrists, and elbow) become hot and swollen. This condition resolves as the disease goes into remission.
Liver disease: in severe attacks of ulcerative colitis, minor elevations in liver enzymes are common and the level returns to normal once remission is achieved. However, in about three percent of patients with ulcerative colitis, a major liver complication can occur in which chronic inflammation of the bile duct can lead to progressive liver disease. The cause of this liver disease is unknown and there is currently no satisfactory treatment for this condition.
Chinese Medicine
TCM identifies ulcerative colitis according to the severity and symptoms exhibited in each individual; these are then allotted into different disharmony patterns or syndromes. Basically, physicians pay special attention to bowel habits such as frequency, quantity, nature, form, color and smell of the stools, as well as the presence of accompanying physical sensations.
Damp-heat in the large intestine
There is usually acute onset of this type. The diarrhea is violent and foul smelling and with a large amount of pus or blood. There is a burning feeling in the anus, abdominal pain and cramps, a rumbling noise and distention that diminishes after defecation. Other accompanying signs are fever or alternating chills and fever, poor appetite, dry mouth, and scanty yellow urine.
Damp-cold in the spleen
Diarrhea with excessive mucus or watery thin stools, tenesmus, abdominal cramps and rumbling noise are also experienced. There are accompanying signs like a bland taste in mouth, stomach stuffiness, no appetite, headache, generalized heaviness, and clear urine.
Qi and Blood stagnation
Diarrhea with alternative solid or loose stools, sticky with mucus or darkish bloody contents; straining to pass a small amount of stools may occur each time; there are also constant stabbing pains at a fixed location that can be aggravated by pressure. Other accompanying signs may be abdominal masses, distention, chest fullness, poor appetite and a darkish facial complexion.
Liver stagnation and spleen weakness
Symptoms are always triggered by emotional stimulation. Usually, diarrhea immediately comes after abdominal cramps; there are loose stools full of mucus with some pus or blood. There are also tenesmus, chest oppression, sighing, irritability, poor appetite and frequent passage of gas. Some individuals may present with alternating diarrhea and constipation.
Spleen qi deficiency
Individuals develop alternating diarrhea and loose bowels, and undigested foods may present in the stools. The loose bowels and frequency are worsened by poor lifestyle habits or consumption of greasy foods. The abdominal cramps are dull in nature and can be relieved by palpation. Other accompanying signs are lack of appetite, gastric fullness after meals, fatigue, sallow complexion, frequent passage of gas, irregular menstruation or even rectal prolapse.
Spleen and kidney deficiencies
Individuals develop a chronic persistent diarrhea that usually contains undigested foods. Diarrhea typically occurs early in the morning after an episode of colic around the navel, and then throughout the day. Other symptoms include fatigue, cold body and extremities, soreness in the lumbar and knees, abdominal dull pain that diminishes with exposure to warmth, profuse clear urine or frequent urination at night.
It should be noted that during the course of ulcerative colitis, the above syndrome patterns may appear alone or in complex form. An experienced physician can accurately identify the pattern.
Ulcerative Colitis : Diagnosis
Western Medicine
The diagnosis of ulcerative colitis is made from the patient's medical history, a stool examination, sigmoidoscopy findings, and biopsy of specimens from the rectum or colon.
Stool Samples
Stool samples from patients with ulcerative colitis contain pus cells, red blood cells, and commonly eosinophils (a type of white blood cells). Since inflammation of the colon due to infections can also produce symptoms similar to those of ulcerative colitis, stool samples are examined to exclude parasitic, amoebic or bacterial infection.
Sigmoidoscopy
Sigmoidoscopy allows the physician to find typical features of ulcerative colitis in the colon, such as swelling, small bleeding points, and ulceration of the inner lining of the colon. For patients with longstanding disease, pseudo polyps may also be seen. Colonoscopy is sometimes necessary for determining the extent of the disease, especially in severe attacks.
Biopsy
Because the findings from sigmoidoscopy can also be found in other medical conditions such as infectious inflammation of the colon, biopsies of the tissue in the colon are necessary to confirm diagnosis of ulcerative colitis. Patients with Crohn's disease can also have a medical history and symptoms similar to those of ulcerative colitis and several biopsies via colonoscopy may be needed to confirm a diagnosis of ulcerative colitis.
Differential Diagnosis
Patients with Crohn's disease, which usually also involves the small intestines, often present with symptoms similar to ulcerative colitis. Endoscopy and x-ray s of the small intestine are sometimes necessary to correctly diagnose ulcerative colitis. Other differences between ulcerative colitis and Crohn's disease are found in laboratory values and biopsy specimens.
Chinese Medicine
In TCM understanding, ulcerative colitis is mainly due to internal weakness of the spleen and stomach that result in transmission disorders of the large intestine. Triggering factors like exogenous pathogens, an improper diet and emotional stimulation further disturb the internal disharmony and make the symptoms worse.
During diagnosis, TCM physicians rely on special skills to gather health information from patients so that appropriate therapeutic strategies can be undertaken.
Damp-heat in the large intestine
TCM diagnostic criteria for this type of ulcerative colitis include diarrhea with pus and blood, a burning feeling in the anus, abdominal cramps, fever and scanty yellow urine. On examination, the tongue is red and covered by yellow greasy coating; the pulse is rolling and rapid.

Damp-cold in the spleen
Diagnostic criteria for this type are diarrhea with mucus or watery stools, tenesmus, abdominal cramps, stomach stuffiness, generalized heaviness and clear urine. On examination, the tongue is pale and covered by white greasy coating; the pulse is hesitant and slow.
Qi and Blood stagnation
Diagnostic criteria for this type of ulcerative colitis include diarrhea with mucus or darkish blood, straining for defecation, fixed stabbing pain, distention, belching and a darkish complexion. On examination, the tongue is purple with bleeding spots; the pulse is taut and hesitant.
Liver stagnation and spleen weakness
Diagnostic criteria for this type of ulcerative colitis includes diarrhea triggered by emotional stimulation; attacks usually come after abdominal cramps, chest oppression, belching and frequent passage of gas. On examination, the tongue fur is thin, white and greasy; the pulse is taut.
Spleen qi deficiency
Diagnostic criteria for this type of ulcerative colitis includes loose bowels made worse by poor lifestyle habits or consumption of greasy foods, undigested foods in the stools, lack of appetite, distention, fatigue and sallow complexion. On examination, the tongue is pale and covered by white fur; the pulse is weak and thready.
Spleen and kidney deficiencies
Diagnostic criteria for this pattern are early morning diarrhea that comes after an episode of colic, undigested food in the stools, cold body and extremities, soreness in the lumbar region and knees, and frequent urination at night. On examination, the tongue is pale; the pulse is deep and thready.
According to TCM experience, damp-heat in the large intestine, qi and blood stagnation, spleen qi deficiency are the most common types of syndrome patterns; while spleen and kidney deficiencies are usually seen in the late stage of ulcerative colitis .
Ulcerative Colitis : Treatment
Western Medicine
The goals of treatment of ulcerative colitis are to induce and maintain remission of symptoms and inflammation of the inner lining of colon. Treatment options are determined according to the extent of the inflammation and the severity of the disease.
5-Aminosalicylic Acid (5-ASA)
The majority of patients with ulcerative colitis have mild or moderate disease with inflammation involving areas close the rectum. In these patients, rectally administered preparation of 5-aminosalicylic acid (5-ASA) is the best treatment option. Rectal preparation of 5-ASA is available as an enema, foam, gel, or suppository, which are equally effective. For patients who prefer oral therapy, sulfasalazine and 5-ASA derivatives (mesalamine, olsalazine, and balsalazide) are also effective in the treatment of mild to moderate ulcerative colitis, although rectal preparations have higher remission and improvement rates.
Sulfasalazine is less effective than corticosteroids for active disease and its major role in the management of ulcerative colitis is to maintain remission once the active inflammation has resolved. However, side effects from sulfasalazine such as headache, nausea, and vomiting can be severe. Rash and infertility in males are also commonly reported with sulfasalazine therapy.
Mesalamine, olsalazine, and balsalazide have been developed to minimize adverse effects seen with sulfasalazine therapy. These new 5-ASA derivatives are shown to be as effective as sulfasalazine in both treating active ulcerative colitis and maintaining remission with fewer side effects.
Corticosteroids
For patients whose symptoms are inadequately controlled with 5-ASA, corticosteroids are used in active disease.
Hydrocortisone is available as an enema, suppository, or foam for rectal administration. For patients with severe ulcerative colitis, oral corticosteroid is used. Prednisone and cortisone are commonly used oral corticosteroids for severe ulcerative colitis but prolonged use can cause many long-term side effects, including osteoporosis and cataract. For patients with severe disease requiring hospitalization, intravenous corticosteroid is also available.
Although corticosteroids deliver fast and reliable remissions of the active ulcerative colitis, these drugs do not change the underlying disease course and they were shown to be ineffective in maintaining long-term remission with continued use. Therefore, corticosteroids should be used to treat active disease and should be used to maintain remission of the disease.
Immunosuppressive Agents
Immunosuppressive agents are often used to allow reduction or elimination of corticosteroids and also to maintain corticosteroid-induced remissions of the disease. The immunosuppressive agents used in ulcerative colitis include azathioprine (AZA), 6-mercaptopurine, and cyclosporine.
Azathioprine and 6-mercaptopurine are most widely used immunosuppressive agents used in ulcerative colitis. These drugs are especially useful in patients who are having repeated relapses from their disease once corticosteroids have been discontinued. It may take up to 6 months for these drugs to achieve a therapeutic effect. Both azathioprine and 6-mercaptopurine are associated with minimal side effects which include nausea, fever, and diarrhea. Pancreatitis and liver dysfunction can also occur and rare occurrence of bone marrow suppression with these drug warrant regular monitoring of blood counts.
Cyclosporine is used for patients hospitalized with severe ulcerative colitis who do not respond to high doses of intravenous corticosteroid s . Although oral formulation of the drug is available, only intravenous administration of cyclosporine has been shown to provide favorable effects in severe ulcerative colitis. It has much faster onset of therapeutic efficacy compared to azathioprine and 6-mercaptopurine, but is not found to be as effective in maintaining remission. Unlike azathioprine and 6-mercaptopurine, cyclosporine is not associated with bone marrow suppression but can cause kidney toxicity.
Surgery
In patient with ulcerative colitis, surgery is performed to remove the colon in the following situations:
- Severe attacks not responding to medical treatment
- Perforation or dilatation of the colon during a severe attack
- Cancer due to ulcerative colitis
Chinese Medicine
TCM believes that the major pathologies of ulcerative colitis include spleen and stomach dysfunctions, intestinal turbid accumulations, and blood and qi disturbances . Therefore, TCM treatment strategies are to restore organ functioning, eliminate turbid accumulations and harmonize the flows of qi and blood.
In clinical applications, if individuals have obvious pus, mucus or bloody loose bowels, physicians will focus on clearing pathogens like damp-heat or damp-cold, so as to improve the bowel environment. Afterwards, tonifying methods are employed to overcome the internal weakness and promote a longer remission period.
I. Herbal prescriptions for UC
Damp-heat in the large intestine
Therapeutic aim: Clearing damp-heat, harmonizing blood and qi.
Sample prescription: Modified Peony Decoction (shao yao tang)
In the prescription, the peony root and angelica root enrich the blood; the betel nut, costus root and rhubarb promote qi flow, the thread rhizome and skullcap root clear damp-heat and detoxify. The whole combination resolves the pathogenic accumulation in the large intestine, enabling the bowel to resume its normal transmission process.

Damp-cold in the spleen
Therapeutic aim: warming and dissolving dampness, harmonizing blood and qi
Sample prescription: Modified Weiling Decoction (wei ling tang)
In the prescription, the atractylodes rhizome and root enhance fluid metabolism in the spleen; the magnolia bark and tangerine peel regulate qi flow to dispel damp-cold; the poria, water-plantain root and chu-ling induce urination; cassia bark and ginger promote warmth to expel coldness. The whole combination enables the intestinal functions to perform normally by enhancing spleen functioning and dispelling damp-cold pathogens.
Qi and Blood stagnation
Therapeutic aim: regulating blood and qi flows to arrest diarrhea and pain.
Sample prescription : Modified Decoction for Removing Blood Stasis in the Lower Abdomen Lower Abdomen Blood Stasis Dispelling Decoction (shao fu zhu yu tang)
In the prescription, the cattail pollen, angelica, lovage and squirrel feces nourish blood and promote tissue regeneration; the corydalis rhizome, peony root and myrrh promote blood and qi flows to arrest pain; the fennel, ginger and cassia bark warm the meridian to dispel blood stasis. The whole combination improves the circulation in the large intestine so as to arrest diarrhea and pain.
Liver stagnation and spleen weakness
Therapeutic aim: soothing liver, invigorating spleen, expelling dampness, arresting diarrhea.
Sample prescription: Modified Essential Formula for Diarrhea with Pain (tong xie yao fang)
In the prescription, the atractylodes root invigorates the spleen; the peony root works on the liver; the tangerine peel regulates qi flow and expels dampness; the ledebouriella root assists the above herbs to work properly. The whole combination invigorates the spleen and expels dampness to arrest diarrhea, soothes the liver and regulates qi to arrest pain.
Spleen qi deficiency
Therapeutic aim: Replenishing qi, invigorating spleen, consolidating intestines to arrest diarrhea.
Sample prescription: Modified Powder of Ginseng, Poria & Atractylodes (shen ling bai shu san)
In the prescription, the ginseng, atractylodes root and poria are the main ingredients to replenish qi and invigorate the spleen; the hyacinth bean, coix seed, lotus seed and yam enhance the water metabolism of the spleen which helps to drain dampness and arrest diarrhea; the amomum fruit promotes the digestive process; the balloonflower regulate the water passages and the liquorice acts as a buffer.
Spleen and kidney deficiencies
Therapeutic aim: warming and tonifying the spleen and kidney, consolidating the intestine to arrest diarrhea.
Sample prescription: Modified Immortal Organ Nourishing Decoction (zhen ren yang zang tang)
In the prescription, the poppy capsule is used in high dosage to consolidate the intestine and arrest diarrhea; cassia bark warms the kidney and spleen; both herbs are the main ingredients. The nutmeg and myrobalan fruit provide warming to arrest diarrhea; the ginseng and atractylodes root replenish qi; the angelica and peony root replenish blood; the costus root and liquorice root act as buffer.
II. Herbal enemas for UC
An enema is the procedure of introducing liquids into the rectum and colon via the anus. Herbal enemas help improve problems affecting the lining of the bowel such as abrasions, edema, ulcers and bleeding, therefore effectively relieving the intestinal symptoms.
Herbal enemas for ulcerative colitis must be carried out in medical or hospital environments. Before the procedure is undertaken, the lower bowel must be cleaned properly; drip a warm herbal preparation slowly into the colon; let the liquid be retained for at least 4 hours so as to obtain the full herbal effects. Do once a day for ten days, and then rest for 4 days before repeating the treatment. Patients usually feel an improvement after 3 courses. Selection of herbs is based on individual cases, below are some suggested ingredients:
Clearing damp-heat accumulation
| bai tou weng | Chinese pulsatilla root | Radix Pulsatillae |
| ye ju hua | wild chrysanthemum | Flos Chrysanthemi Indici |
| pu gong ying | dandelion | Herba Taraxaci |
| huang lian | golden thread rhizome | Rhizoma Coptidis |
| bai jiang cao | patrinia | Herbal Patriniae |
Removing blood and qi stagnation
| dan pi | peony tree root bark | Crotex Moutan Radicis |
| huang qin | baical skullcap root | Radix Scutellariae |
| huai hua | pagoda tree flower | Flos Sophorae |
| san chi | notoginseng | Radix Notoginseng |
| da huang | Chinese rhubarb | Radix et Rhizoma Rhei |
Soothing liver and invigorating spleen
| bai ji | common bletilla tuber | Rhizoma Bletillae |
| chai hu | bupleurum root | Radix Bupleuri |
| bai shao | white peony root | Radix Paeoniae Alba |
| yu jin | turmeric root tuber | Radix Curcumae |
| wu yao | lindera root | Radix Linderae |
Tonifying spleen and stomach
| huang qi | astragalus | Radix Astragali |
| dang shen | pilose asiabell root | Radix Codonopsis Pilosulae |
| bai shu | largehead atractylodes root | Rhizoma Atractylodis Macrocephalae |
| chen pi | dried tangerine peel | Pericarpium Citri Reticulatae |
| dang gui | angelica root | Radix Angelicae Sinensis |

III. Acupoint therapies for UC
Stimulation of acupoints not only enhances the immune modulation effect, but also mobilizes the innate healing power inside the body. For the localized problems like inflammation, ulcers, muscular spasms and sluggish flow, acupuncture and moxibustion are particular effective and thus facilitate structural recovery.
Suggested acupuncture methods:
Major points: navel's four-point (one-thumb-width apart from the navel, located in three, six, nine & twelve o'clock), tian-shu, guan-yuan & qi-hai;
Assist points: da-chang-shu, zhang-qiang, pi-shu, wei-shu, zu-san-li & san-yin-jiao.
When applying, first punch the four-point needle in 0.3-0.5 cm deep and rotate for about 30 seconds, stimulate the four locations in a clockwise sequence, no needle retention; then select one more major point and 2-3 assist points for stimulation, retain the needles on the locations for 15-20 minutes, moxa cones can be attached for heating during this time. Do this once daily or every two days, ten times is one course.
Moxibustion can also be used to boost the weakened systems, particularly for individuals with chronic symptoms. Below are suggested protocols:
Major points: zhong-wan, tian-shu, guan-yuan & shang-ju-xu;
Assist points: pi-shu, shen-shu, da-chang-shu, zu-san-li, tai-xi, tai-chong, san-yin-jiao & zhong-iv-shu.
Each time, select 1-2 major points and heat for 30-40 minutes; while select 2-3 assist points and heat for 15-20 minutes. Do this once daily or every two days, 15-20 times is one course.

Acupoints for UC
Ulcerative Colitis : Prevention
Western Medicine
There are no known preventative measures for ulcerative colitis. However, approximately seventy percent of patients with ulcerative colitis are expected to experience relapse of the disease over a twelve-month period; acute attacks or flare-ups can be prevented by adhering to maintenance therapy with 5-ASA and azathioprine or 6-mercaptopurine.
Chinese Medicine
Since ulcerative colitis has no definitive preventive measures, TCM's goal is to extend the remission period in affected individuals. An optimistic and calm emotional state and healthy life habits are crucial for preventing relapse or further aggravation. See "Good Life Habits and Mind Cultivation". In addition, TCM highly recommends dietary restraint - the diet should consist of easily digested foods. The intestinal symptoms may be alleviated by avoiding fresh fruits and vegetables, caffeine, alcohol, spicy and greasy foods.
For acute relapse patients who suffer from loose bowels with excessive amount of pus, mucus or blood, it is helpful to eat a certain amount of ingredients to clear the accumulated pathogens. For example, suggested foods for obvious mucus watery diarrhea are crucian carp, pepper, ginger, nutmeg and lesser galangal rhizome; foods for foul pus diarrhea are cucumber, purslane, hyacinth beans and rice beans; foods for dark bloody diarrhea are black beans, brown sugar, safflower, tangerine peel and hawthorn fruit .
For chronic ulcerative colitis sufferers, tonic foods like yams, hyacinth bean, poria, red dates, lily buds, coix seeds, euryale seeds, lotus seeds and wolfberry fruit can boost the weakened organs and help to restore normal bowel movements.
Below are sample recipes:
Clearing damp-heat
Purslane (fresh 120g / dried 60g), mung beans (60g); decoct and take once a day for one week.
Chinese pulsatilla root (50g), honeysuckle flower (30g) and silk cotton flower (30g); decoct and add sugar to taste; take once a day for one week.

Arresting chronic and persistent diarrhea
Lotus seeds (30), euryale seeds (30) and rice (30g); cook into porridge, add sugar to taste and serve as breakfast.
Fresh yam (500g), mutton (250g) and glutinous rice (250g); first stew the yam and mutton to fully tender, and then add to the rice and water for further cooking into porridge.
Psoralea (10g) and one pig kidney; wash the ingredients thoroughly, stew for 2 hours on a simmering heat, add salt to taste. Drink the soup and eat the kidney.
Ulcerative Colitis : References
Western Medicine References
- Korbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults. The American Journal of Gastroenterology. 1997; 92(2): 204-211.
- Podolsky DK. Inflammatory bowel disease. New England Journal of Medicine. 2002; 347(6): 417-429.
- Gionchetti P, Amadini C, Rizzello F, et al. Treatment of mild to moderate ulcerative colitis and pouchitis. Alimentary Pharmacology and Therapeutics. 2002; 16 (Suppl 4): 13-19.
- Kamm MA. Maintenance of remission in ulcerative colitis. Alimentary Pharmacology and Therapeutics. 2002; 16 (Suppl 4): 21-24.
- Daperno M, Sostegni R, Rocca R, et al. Medical treatment of severe ulcerative colitis. Alimentary Pharmacology and Therapeutics. 2002; 16 (Suppl 4): 7-12.
- Nicholls RJ. Ulcerative colitis – surgical indications and treatment. Alimentary Pharmacology and Therapeutics. 2002; 16 (Suppl 4): 25-28.
- Jewell DP. Ulcerative Colitis. In: Feldman M, Scharschmidt BF, Sleisenger MH, Klein S, et al, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease, Edinburgh: Saunders Company, 1998.
Written By:
Jiwon Kim, Pharm.D.
Assistant Professor of Clinical Pharmacy, University of Southern California School of Pharmacy
- Li gan-gou & Wang Zi-li. TCM Gastroenterology, China Medicine and Technology Publishing House, 1993.
- Zhou Wen-quan et al, chief edited. Chinese Medicinal Diet – Syndrome Differentiation Therapies, Beijing: People's Medical Publishing House, 2000.
- Wang Tai-kang chief edited. TCM Treatment for Complex and Miscellaneous Diseases, China Medicine and Technology Publishing House, 2002.
- http://www.cintcm.com
Written By:
Dang Yi, PhD.
Professor, Beijing University of Chinese Medicine
Editors:
Jennifer Eagleton, BA, MA (Asian Studies), Integrated Chinese Medicine Holdings Ltd. Rose Tse, Integrated Chinese Medicine Holdings Ltd.